In 2018, a study published in the American Journal of Obstetrics and Gynecology (AJOG) found that 61,174 singleton pregnancies were used in prospective research data to identify high-risk pregnant women using maternal factors combined with PLGF testing before proceeding to the second stage Detection and screening of preeclampsia can effectively predict the occurrence of about 90% of preeclampsia, while reducing unnecessary expenditures and improving economic benefits.
Research Background
Dr. Alan Wright and colleagues from the University of Exeter in the United Kingdom wrote in the article that during pregnancy,From 11 to 13 weeks, the "triple detection" of maternal factors combined with mean arterial pressure (MAP), uterine artery pulsatility index (UtA-PI) and serum placental growth factor (PLGF) can predict about 90% of preeclampsia. They also pointed out that it is necessary to screen for preeclampsia in the first trimester, because if high-risk pregnant women take aspirin before 16 weeks of gestation, the incidence of early-onset preeclampsia (delivery less than 32 weeks) can be reduced by 90%, making premature delivery. The incidence of preeclampsia (delivery less than 37 weeks) is reduced by 60%.
However, the article stated that serum PLGF and UtA-PI,the measurement is not part of the routine pregnancy test and requires additional costs. Therefore, whether the experimental study can pass the two-stage screening strategy can not only maintain the original detection efficiency, but also reduce unnecessary detection and improve economic benefits.
Research methods
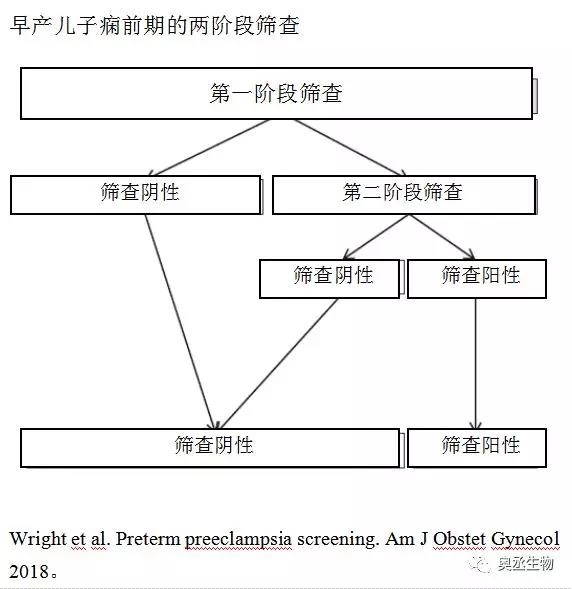
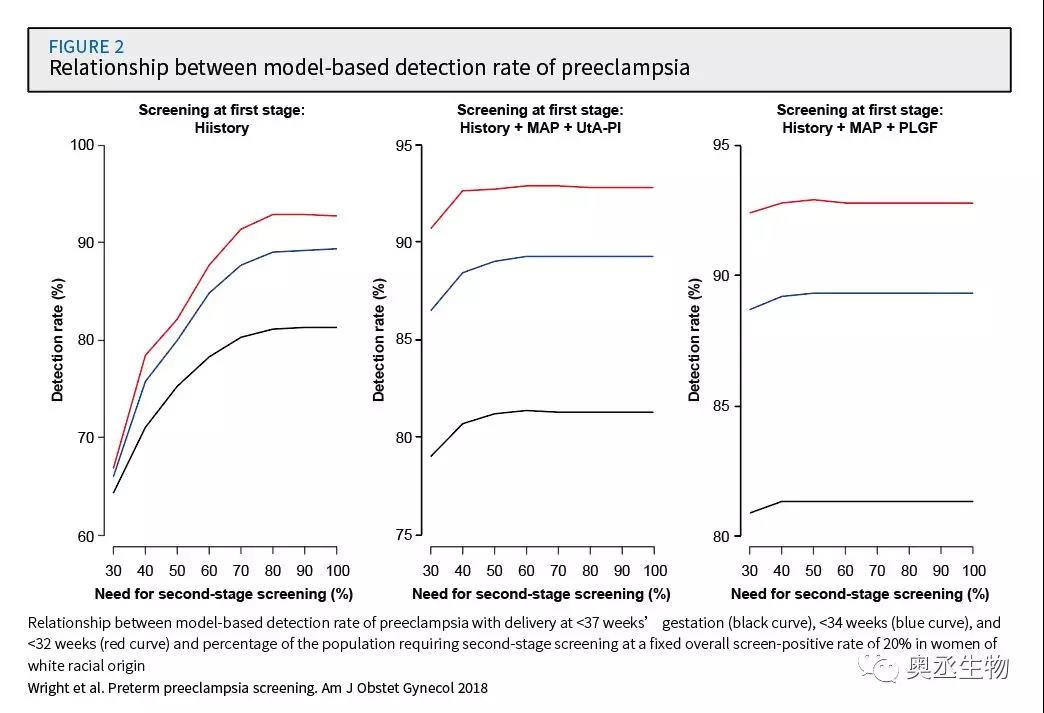
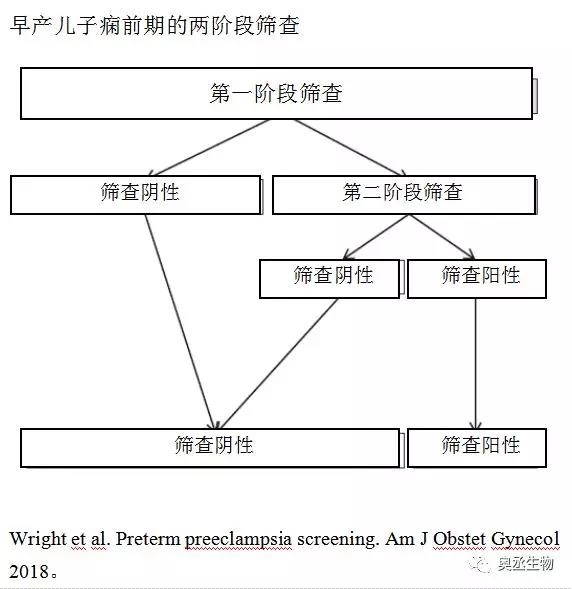
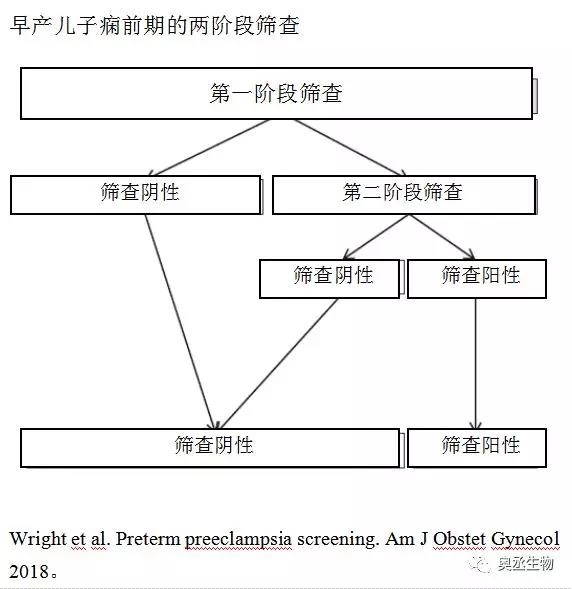
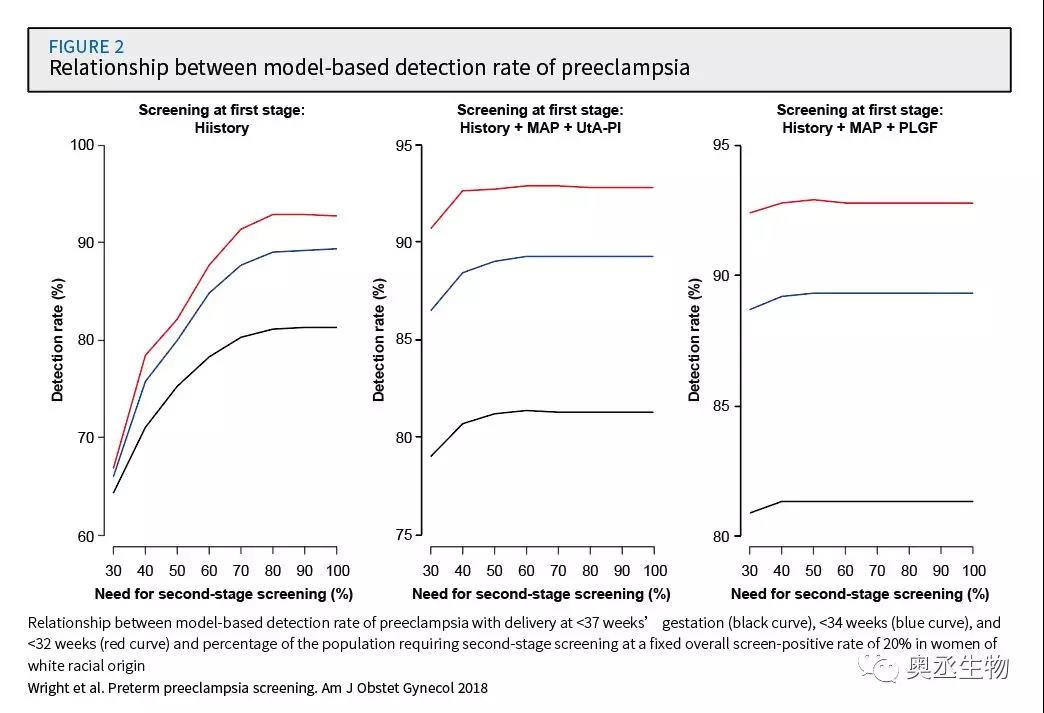
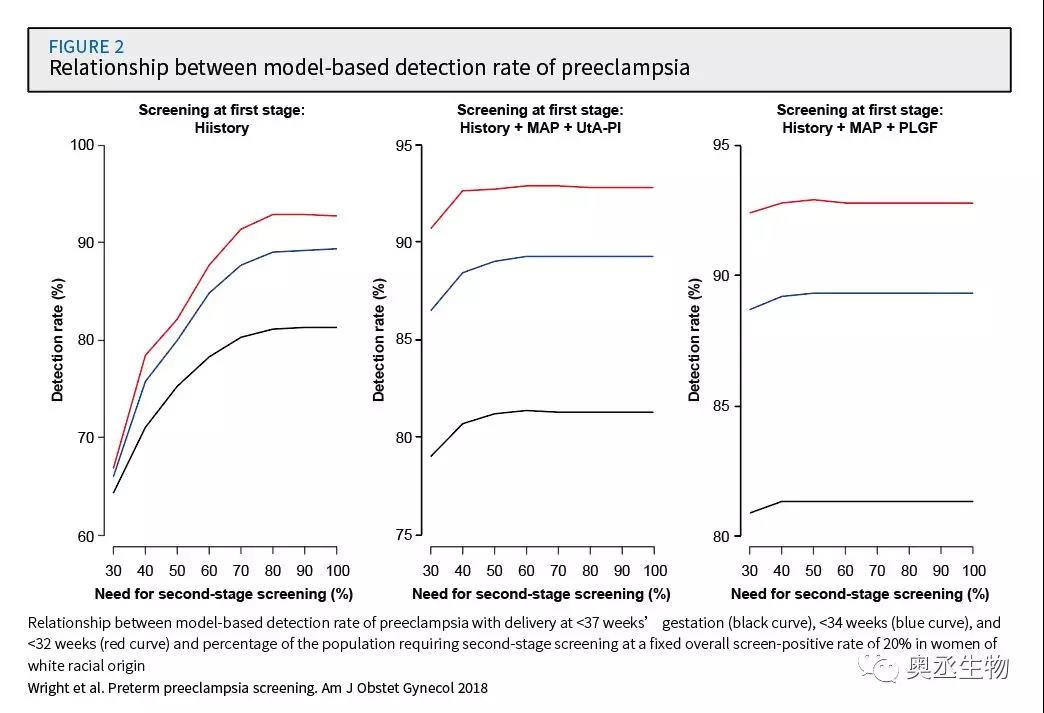
In this study, the researchers used a risk competition model to conduct the first stage screening through maternal factors/maternal factors, MAP and UtA-PI/maternal factors, MAP and PLGF, and then screened high-risk pregnant women in the second stage Perform a complete triple test. Compare different screening methods to screen the effects of preeclampsia.
Research result
The results of the experiment found that if the first stage of screening is combined with maternal factors, MAP and UtA-PI, the number of pregnant women who need PLGF testing can be reduced to 30%-40%. Similarly, if the first stage of screening is combined with maternal factors, MAP and PLGF, the number of pregnant women who need UtA-PI testing can be reduced to 20%-30%. And the two-stage screening strategy is similar to that of all pregnant women. The detection rate of preeclampsia is similar.
The researchers said, "There is no doubt that testing only a part of the population will be more economical than testing all the population." The results of the study prove that the use of maternal factors combined with PLGF testing to identify high-risk populations for further screening The effectiveness of the two-stage preeclampsia screening strategy.